What is the Ohio Behavioral Health Integrated ODMH/ODADAS Discharge Form?
This form is used to summarize a client's treatment episode and discharge status from a behavioral health service. It includes information such as the provider number, client details, discharge reason, and additional data regarding education, income, living arrangements, substance use, and health conditions.
Who should complete this discharge form?
Healthcare professionals within the Ohio Department of Mental Health and Addiction Services (ODMH/ODADAS) network responsible for a client's care are required to fill out this form at the point of discharge. This includes clinicians or administrators overseeing the client's treatment plan and discharge process.
What are some of the key reasons for discharge listed on the form?
The form outlines various reasons for discharge, including successful completion, client left on own against staff advice, involuntary discharge due to non-participation or violation of rules, referral to another program, incarceration, transfer for health reasons, death, client moved, needed services not available, and other reasons not specified.
Does the discharge form cover substance use information?
Yes, it includes sections for identifying a client's primary, secondary, and tertiary drug of choice, the frequency of use, route of administration, age of first use or intoxication, and whether the client uses tobacco products.
How is a client's physical health addressed in the form?
It requires reporting on any significant physical health conditions the client has experienced in the past year, such as diabetes, high cholesterol, cardiovascular disease, high blood pressure, cancer, kidney disease, or any respiratory diseases.
What does the form say about a client's living arrangements?
The form requests information regarding the client's living situation at discharge, including independent living, homelessness, residence in a treatment or care facility, or other arrangements.
Are details regarding a client's education and employment included?
Yes, the form collects data on the highest level of education completed, current employment status, type of primary income or support, and whether the client is engaged in educational enrollment at the time of discharge.
What about mental health diagnoses?
The form allows for the listing of primary, secondary, and tertiary DSM IV or ICD9 mental health condition diagnoses, which helps to provide a comprehensive view of the client's mental health status at the time of discharge.
How does the form address client’s engagement in self-help or community support programs?
It includes a section to indicate the frequency of the client's attendance at self-help or community support programs in the 30 days prior to discharge, which could range from no attendance to daily participation.
Is client reimbursement or insurance information required?
Yes, the form requires information on the primary source of reimbursement for the client's treatment, including self-pay, insurance types (like Medicaid, Medicare, Blue Cross/Blue Shield), or other government support.
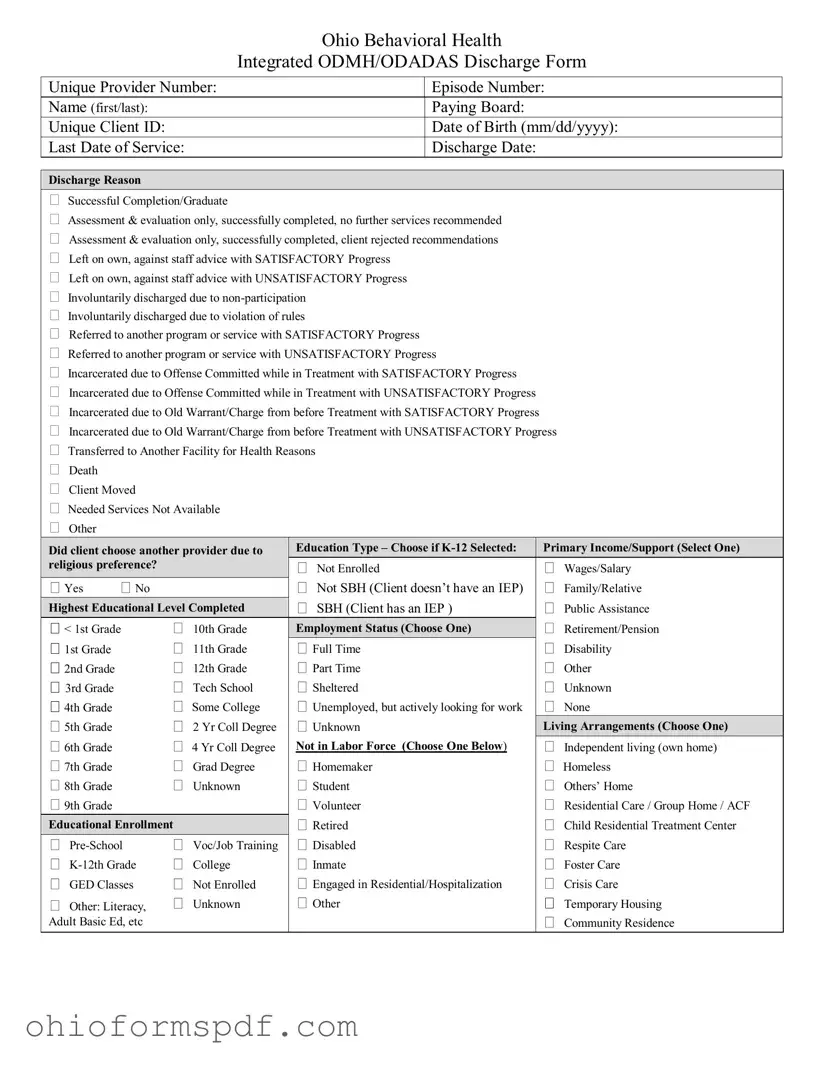
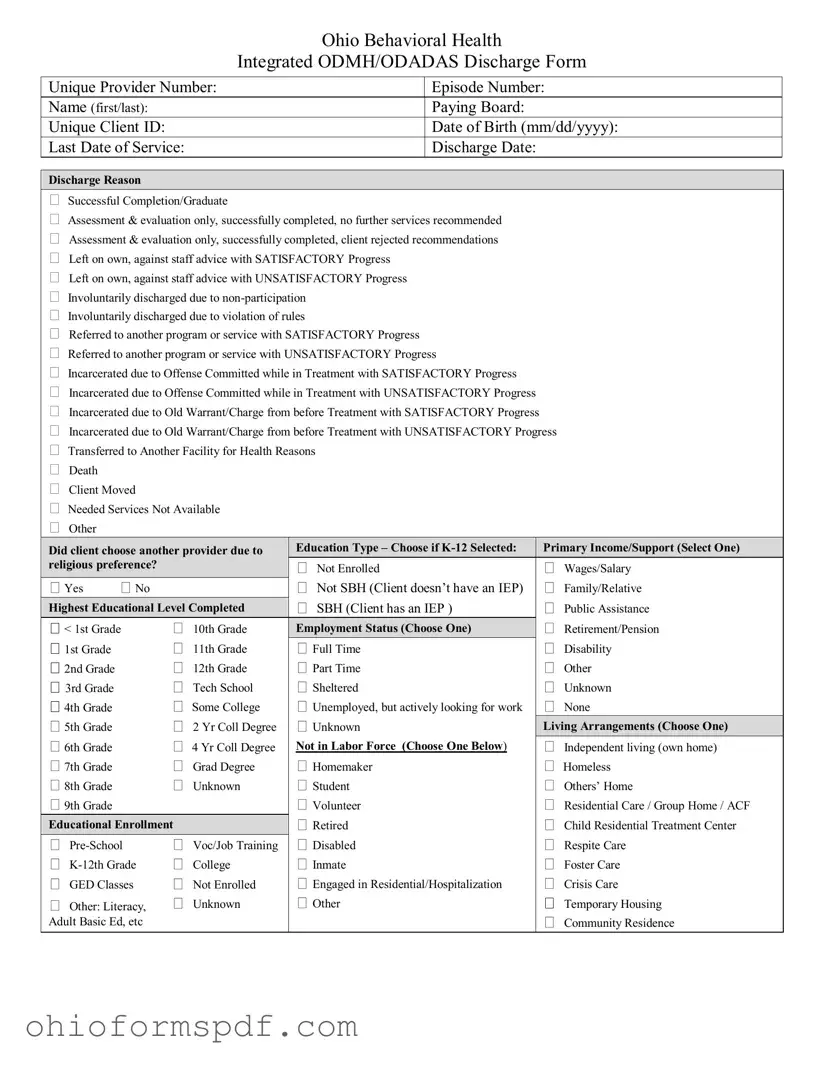
 Discharge Reason
Discharge Reason