The Ohio Odm 02374 form shares similarities with the Request for Medicaid Prior Authorization forms used by other states. These forms, often required for various types of services beyond private duty nursing, play a key role in the Medicaid program by managing costs and ensuring the provision of necessary medical services. Like the Ohio Odm 02374, these forms require detailed patient information, provider details, and a thorough description of the requested service to be considered for approval.
Forms similar to the Ohio Odm 02374 include Home Health Services forms, which request approval for services provided in a patient's home, such as physical therapy, occupational therapy, and home health aide services. Although focusing on a broader range of services, these forms also ask for patient demographics, diagnosis, and medical necessity justification—elements crucial for determining the appropriateness and extent of services authorized.
Waiver Service Authorization forms, designed to obtain approval for services covered under Medicare waivers, notably resemble the Ohio Odm 02374. These waivers allow for the provision of long-term care services in home and community-based settings rather than institutional settings. The requirement for detailed consumer and provider information, alongside a detailed service plan, mirrors the structure of the Ohio form.
Durable Medical Equipment (DME) Prior Authorization forms also share similarities with the Ohio Odm 02374. These forms are necessary for obtaining approval for medical equipment that is essential for the patient's daily life. Like the Ohio form, DME forms require specifics about the patient’s medical condition and the necessity of the equipment, in addition to provider information to facilitate the approval process.
Pharmacy Prior Authorization forms are required for Medicaid programs to approve certain prescribed medications not covered under the state's preferred drug list. Similar to the Ohio Odm 02374, these forms necessitate detailed information about the patient, the prescribing provider, and a clinical rationale for the requested medication, highlighting the intersection of patient care coordination and medication management.
The Facility-Based Service Request forms, utilized for services provided in a facility such as a nursing home or rehabilitation center, align with the Ohio Odm 02374 in their comprehensive collection of patient and facility provider information. Ensuring Medicaid patients receive appropriate care, these forms parallel the individualized care approach seen in private duty nursing requests.
Prior Authorization Request forms for Specialty Services, such as physical therapy, speech therapy, or other specialized care, necessitate detailed information on the beneficiary’s condition and the expected outcomes of the therapy, akin to the Ohio Odm 02374 form. They play a pivotal role in managing the provision of specialized services within Medicaid's framework.
Behavioral Health Services Authorization forms, which are essential for accessing mental health and substance abuse treatment services, echo elements of the Ohio form through their requirements for thorough patient assessments, treatment plans, and provider credentials. This similarity underscores the comprehensive approach needed to address diverse patient needs across healthcare domains.
Transportation Service Authorization forms, necessary for approving non-emergency medical transportation services for Medicaid beneficiaries, share the need for detailed beneficiary information and medical necessity justification found in the Ohio form. These forms ensure that transportation barriers do not impede access to critical healthcare services.
Finally, the Pediatric Palliative Care Authorization forms, required for pediatric patients needing specialized palliative care services, resemble the Ohio Odm 02374 in their focus on detailed patient and care provider information. These forms emphasize the need for a holistic approach to care planning and authorization in sensitive and complex medical situations.
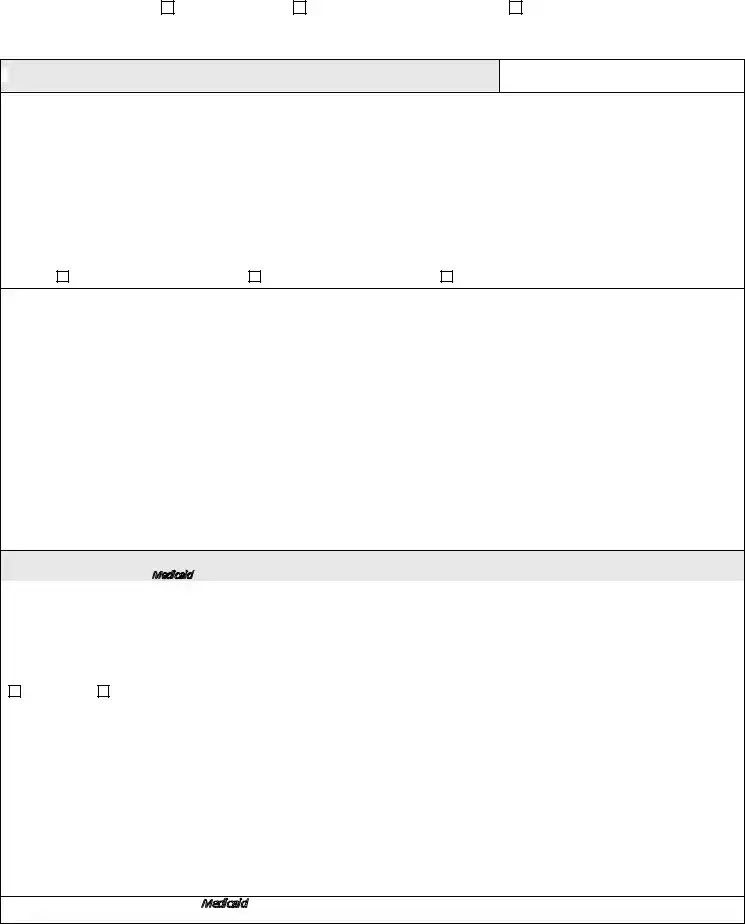

 REQUEST FOR PDN SERVICES BEYOND THE
REQUEST FOR PDN SERVICES BEYOND THE  NOTIFICATION OF PROVISION OF EMERGENCY SERVICES
NOTIFICATION OF PROVISION OF EMERGENCY SERVICES